Table of Contents
As you may already know (from your own painful experience and often fruitless research), the medical circle has a tough time to define vulvodynia.
One thing they do seem to agree upon is that this isn’t a simple gynecological condition and that the solution doesn’t lie in a one-size-fits-all approach.
#1: What Is Vulvodynia?
Vulvodynia is a chronic pain condition affecting the vulva (yep, if you are the proud owner of female reproductive organs then this is the area that can be seen between your legs – also called external genitalia or the vulvar area).
Vulvodynia is a type of vulvar pain that lasts at least 3 months, occurs without a clearly identifiable cause (it can’t be explained by another health problem), with the absence of any visible abnormalities (the affected vulva looks normal), and which may have potential associated factors.
#2: Vulvodynia Symptoms
Chronic vulvar pain is mostly described as burning, however, each person can experience pain differently. Some describe the pain also as stinging, aching, throbbing or itching. Other sensations often mentioned are soreness, rawness, irritation or feeling swollen.
#3: Types of Vulvodynia
Nowadays, to characterize the types of vulvodynia, the medical community uses a pain-based system. Vulvodynia can affect your entire vulva or the pain can devour different parts of it, each with distinct intensities, durations, and onset.
The type of pain is characterized by:
Location of Pain
1. Localized Pain – localized pain occurs in a specific vulvar area:
- Vestibule called Vestibulodynia
- Perineum
- Clitoris called Clitordynia
- Urethra
- Rectum
- Anus
- Labia
- One side of the vulva called Hemivulvodynia
- And even upper leg and thigh!
- Some women also have pain when they empty their bowels
2. Generalized Pain – generalized pain is diffused. It occurs in many or all of the above-mentioned parts of your vulva.
3. Mixed Pain – localized and generalized pain occurs at the same time.
What Elicits the Pain
1. Provoked Pain – pain is provoked when pressure is applied to the vulvar area. Which can happen at any time and anywhere, if you:
- Wear fitted pants (e.g., jeans)
- Sit for an extended period of time (at work, school, cinema, etc.)
- Insert a tampon
- Have sex
- Have a gynecological exam
- Exercise (e.g., biking)
2. Spontaneous Pain – pain just happens, without any pressure
3. Mixed Pain – provoked and spontaneous pain happens together
The Pattern of Pain
- Intermittent
- Persistent
- Constant
- Immediate
- Delayed
Onset of Pain
1. Primary – the pain has been there since first intercourse which means that the person has never experienced pain-free sex
2. Secondary – there was a period of pain-free sex before the pain hit
Based on this pain-based system used to characterize vulvodynia, there are two major subtypes of vulvodynia:
PVD - PROVOKED VESTIBULODYNIA
Formerly called vulvar vestibulitis or vestibulodynia – the most common and well-recognized subtype of vulvodynia, which is localized and characterized by pain at the vaginal opening called vestibule. Pain is provoked by sex, tampon insertion, gynecological exam, exercising, and wearing tight clothing. The vestibule might appear inflamed and red. It is also described as primary or secondary.
GVD - GENERALIZED VULVODYNIA
Formerly called essential or dysesthetic vulvodynia – is characterized by unprovoked, spontaneous, diffused pain, spread out throughout the entire vulva. Pain may be constant or intermittent.
#4: Vulvodynia Diagnosis and Examination
Vulvodynia doesn’t have identifiable causes, nor externally visible symptoms. On top of that, a doctor’s exam can appear completely normal. Because of this, vulvodynia is often either undiagnosed or misdiagnosed.
It is rather “normal” that you may seek help from many health care providers (like gynecologists, family doctors, dermatologists, urologists, alternative health practitioners, etc.). They are usually not familiar with this condition, or even if they are – they don’t know what to do with it.
In the end, many of us, simply stop seeking help. Because it seems frankly pointless.
Vulvodynia Diagnosis
Diagnosis of vulvodynia is a diagnosis of exclusion.
If your doctor can define the culprit of your vulvar pain through proper diagnosis, and then resolve it via adequate treatment (which eventually makes you pain-free) then YOU DON’T SUFFER FROM VULVODYNIA. You suffer from vulvar pain secondary to (a.k.a. caused by) whichever condition you were treating for. Like lichen sclerosus, for example.
However, if a cause of your pain can’t be found and you are still in pain, despite various diagnoses and treatments, then your doctor is able to label your pain as vulvodynia.
Additionally, vulvodynia can also co-exist with other vulvar conditions. Which means that you can suffer from vulvar pain caused by contact dermatitis (for example) and vulvodynia at the same time.
On top of this, the medical community is slowly starting to understand that vulvodynia might be a multifactorial condition – caused by more that one single culprit.
Vulvodynia Examination
There are no specific tests to diagnose vulvodynia. Diagnosis is made based on the exclusion of other vulvar conditions.
You can find examples of the types of examinations used to assess vulvodynia below:
1. Verbal Assessment
- Your doctor can ask you, among other things, about your:
- General health
- Health problems (medical and medicine history)
- Sexuality and sexual history
- Pain symptoms
2. Q-Tip/Cotton Swab Test
- During this test, the doctor will touch different areas on and around your vulva to see how bad your pain is.
3. Physical/Pelvic Exam
- The doctor will assess your external genitals and internal pelvic structure for signs of infection, skin problems or other causes of your symptoms.
4. Pap-Smear
- The doctor can take a culture from your vagina to rule out problems like sexually transmitted diseases or infections.
5. Biopsy
- If during the Q-tip test or pelvic exam, the doctor notices any skin changes or visible problems then she/he can remove a small piece of tissue from your vulva to send to the lab to find out what the problem might be.
6. Colposcopy
- During this examination, the doctor uses a special magnifying device called a colposcope – that allows her/him to closely examine your cervix, vagina and vulva for any signs of disease.
#5: Vulvodynia Causes
According to Western Medicine, vulvodynia has no identifiable cause. Because of this, there are a lot of tags that might get stuck to your condition. One of them is still relatively widespread: “it is all in your head” (my favorite, of course).
Potential Associated Factors with Vulvodynia
Vulvodynia is an idiopathic condition. However, the fact that your vulva appears normal does not mean that there is no cause for the discomfort. It simply has not been identified by the doctors yet!
However, potential associated factors now being defined by the medical community are the first steps into concrete progress in research about vulvodynia!
Why? Because before the 2015 classification (when vulvodynia terminology was updated based on new findings), sufferers were left alone with absolutely nothing regarding the etiology of their condition.
Below, you can find the potential associated factors that may cause your vulvodynia:
- Co-morbidities (co-existing conditions) and other pain syndromes like painful bladder syndrome, fibromyalgia, irritable bowel syndrome, temporomandibular disorder
- Genetic factors such as increased susceptibility to chronic vestibular inflammation and hormonal changes caused by contraceptive pills (for example), or the inability to combat vulvovaginal infections
- Hormonal factors like an inadequate amount of estrogen
- Inflammation caused by elevated levels of inflammatory substances in the vulvar tissues after recurrent infections
- Musculoskeletal, like pelvic muscle overactivity or weakness
- Neurological mechanisms:
- Central (spine, brain)
- Peripheral (hyperinnervation) – characterized by the increased density of the nerve fibers in the vulvar vestibule
- Psychosocial factors like mood, anxiety, stress
- Structural defects like perineal descent or pelvic organ prolapse
Vulvar Pain Causes
If the cause of your vulvar pain is possible to define and resolve, then YOU DON’T SUFFER FROM VULVODYNIA. You suffer from vulvar pain secondary to (a.k.a. caused by) whichever condition you were treating for.
Vulvar pain (not vulvodynia) is an obvious and often visible symptom of some other problem going on in your body and there are many diseases that can cause it.
Below, you can find some conditions that may cause your vulvar pain:
- Infections
- Recurrent yeast infections (e.g., candida)
- Recurrent bacterial, viral or parasitic infections (e.g., B-step, Shingles, Herpes, Cytolic Vaginosis, Trichomonas)
- Disturbed body pH balance due to frequent antibiotic use
- Allergies or sensitivities to chemicals, food, or other substances
- Skin irritations like contact dermatitis of the vulva (from using soap, pads, toilet paper, etc.)
- Inflammations caused by a weakened immune system including disorders like lichen sclerosis or lichen planus of the vulva
- Neoplastic diseases like Paget disease, squamous cell carcinoma
- Neurological issues caused by nerve irritation or injury like post-herpetic neuralgia, neuroma, pudendal nerve entrapment or pudendal neuralgia
- Trauma like female genital cutting, obstetrical issues, sexual abuse
- Iatrogenic issues like post-operative, chemotherapy, radiation
- Hormonal problems and deficiencies like lactational amenorrhea, vulvovaginal atrophy from a low level of sex hormones, use of oral contraceptive pills
- Pelvic floor muscle spasm, tension, or weakness
#6: Vulvodynia Treatment
Based on research, the medical community is starting to acknowledge that vulvodynia might be a multifactorial condition – caused by more that one single culprit.
Because of this, the cookie-cutter approach is not the way to go anymore. Not everyone needs surgery or even physical therapy!
Your treatment should be chosen accordingly, based on your specific case of vulvodynia and your individual needs. The typical treatment plan is based on “trial and error.” It usually starts with non (or less) invasive treatments and based on results, is escalated to more invasive ones.
The important thing to remember is that because of the tricky nature of this condition, in most cases only a multi-disciplinary approach can give lasting results.
There are two main and significantly different directions which you might want to explore during your journey with vulvodynia: the traditional medicine approach, and the complementary and alternative medicine approach.
The first – traditional medicine – approach includes:*
- Antidepressants
- Anticonvulsants
- Topical medication (e.g., topical hormonal creams, topical anesthetics, topical antifungal creams)
- Pain medication like opioids
- Antibiotics
- Antivirals
- Nerve blocks
- Neurostimulation and spinal infusion pump
- Mona Lisa Touch
- Botox
- Surgery
The second – complementary and alternative medicine – approach includes*:
- Counseling and psychological therapies
- Discontinuation of all types of irritants (e.g., soaps, pads, toilet papers)
- Pelvic Floor Muscle Therapy
- Dilator therapy
- Biofeedback
- Icing or heating (ice packs or heat pads)
- Diet changes and modifications
- Natural antifungal and antibacterial oral and topical treatments
- Sitz baths
- Nutritional supplementation
- Stress management
- Meditation
- Developing mind-body connection
- Self-development
- Emotional healing
- Acupuncture
- Reiki
- Qigong
*These lists are not exhaustive.
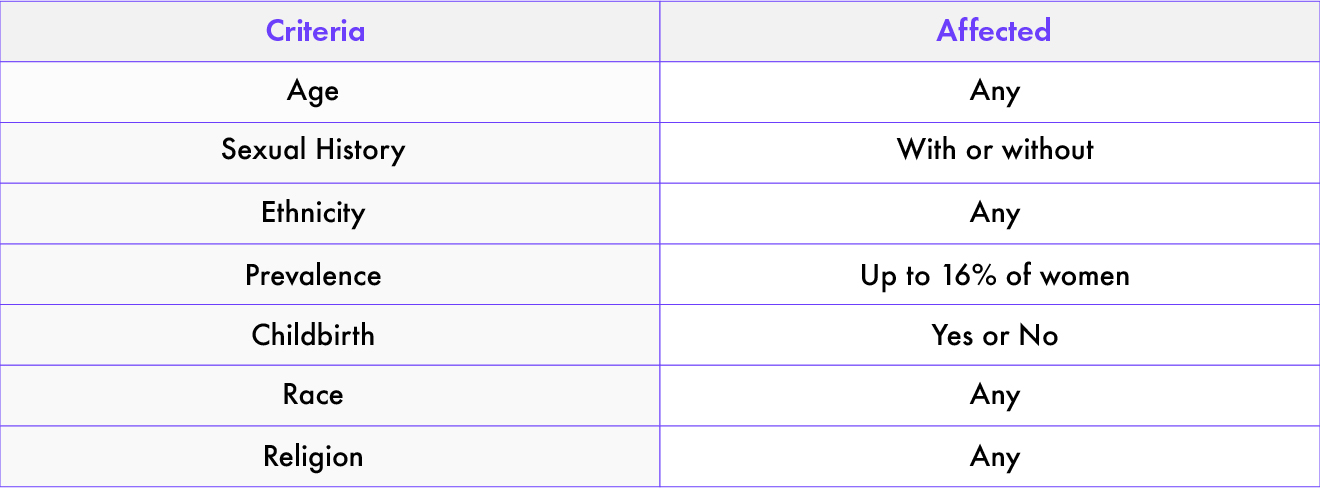
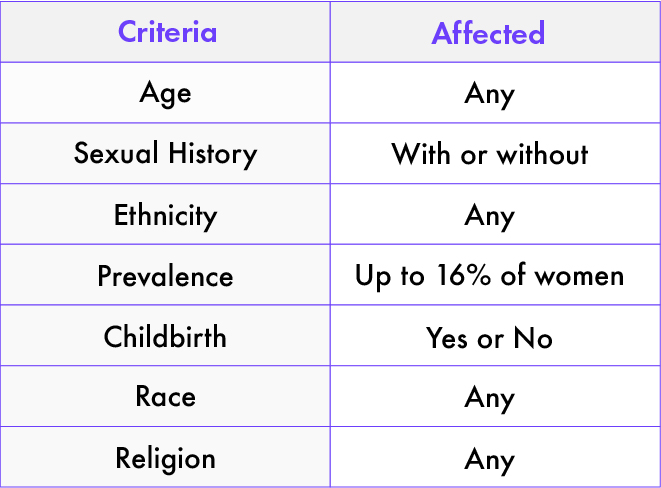
#7: Who Does Vulvodynia Affect?
In the past, doctors believed that vulvodynia is a rare condition. But as research is showing right now, it simply has been under-recognized.
Vulvodynia affects many. The estimates of how many women and girls are affected vary, but in all cases, the number is huge, reaching even up to 16% in women between the ages of 18 and 64.
And not only that, vulvodynia is completely non-discriminatory. It affects women and girls of all ages, ethnicities, backgrounds, etc.
#8: What is Vulvodynia - Not?
To set the record straight (as we’ve all heard a lot of terrifying accusations) and make the case clear (so we never again doubt this topic), it’s useful to mention what vulvodynia is not.
- Vulvodynia is not an STD
- Vulvodynia is not contagious (you cannot pass it on to your partner)
- Vulvodynia is not cancer
- Vulvodynia is not hereditary
- Vulvodynia is not an infection
Conclusion
Hopefully, this post answers some of the initial questions that you might have had:
-
- What is vulvodynia and what are its symptoms, types
- What is the difference between vulvodynia and vulvar pain
- What could be the potential causes of vulvodynia and how to diagnose and examine it
- What are some available treatments
Did you find this post helpful? If yes, what other types of information would you like me to share with you? How can I improve this post?
Hey, Vulva Warriors!
Are you someone who suffers from vulvodynia (chronic vulvar pain)? How do you manage it? How did you find out that you have vulvodynia? Which doctor(s) helped you to diagnose this condition and go through it? Would you like to share your personal insights to help others through their tough journey?
If you would like to share your thoughts, experiences, and questions or simply say hi, please feel free to contact me through the comment section below, on FB or at community@meandmyv.com.
Hello, Health Professionals!
If you are a health professional that deals with vulvodynia you would like to share your experience, cooperate, simply connect or drop a question, please feel invited to contact me through the comment section below, on FB or at community@meandmyv.com.
Disclaimer
My goal is to provide you with the most relevant and current information that is factually correct, comprehensive and up-to-date.
However, the information provided herein might be subject to changes and is not intended to cover all possible:
-
- Vulvodynia symptoms and types
- Vulvodynia diagnosis and examination
- Vulvodynia causes and treatments available
Please also bear in mind, that this article should not be used as a substitute for the knowledge and expertise of a doctor or other licensed healthcare professionals. Please, before taking any medication, consult with your health provider who knows your medical history.
Resources
-
- Sadownik, Leslie A. “Etiology, Diagnosis, and Clinical Management of Vulvodynia | IJWH.” Journal of Pain Research, Dove Press, 2 May 2014, www.dovepress.com/etiology-diagnosis-and-clinical-management-of-vulvodynia-peer-reviewed-article-IJWH.
- Henzell, Helen,Berzins, Karen. “Localised provoked vestibulodynia (vulvodynia): assessment and management”, RACGP, July 2015, https://jeanhailes.org.au/contents/documents/Health_Professionals/Webinars/Vulvodynia.pdf
- “Vulvar Conditions & Management: An Educational Booklet for Patients”, 2017, https://medicine.umich.edu/sites/default/files/content/downloads/Vulva%20patient%20hand%20out%20final%20update%20Jan%202017.pdf
- “Vulvodynia.” Mayo Clinic, 22 July 2017, www.mayoclinic.org/diseases-conditions/vulvodynia/symptoms-causes/syc-20353423
- “Vulvodynia.” Eunice Kennedy Shriver National Institute of Child Health and Human Development, U.S. Department of Health and Human Services, www.nichd.nih.gov/health/topics/vulvodynia
- Skarnulis, Leanna. “Chronic Vulva Pain Management.” WebMD, www.webmd.com/sex-relationships/features/managing-chronic-vulva-pain#4
- Jantos, Marek. “A Psychophysiological Perspective on Vulvodynia.” University of Adelaide, June 2016, https://digital.library.adelaide.edu.au/dspace/bitstream/2440/61980/8/02whole.pdf
- Bornstein, Jacob MD. “The Consensus Terminology of Persistent Vulvar Pain and Vulvodynia.”, Galilee Medical Center, Department of Obstetrics & Gynecology, http://www.pelviperineology.org/march-2018/pdf/consensus-terminology-persistent-vulvar-pain-and-vulvodynia.pdf
- Bornstein, Jacob MD, Goldstein, Andrew MD, Coady, Deborah MD. “2015 Consensus terminology and classification of persistent vulvar pain”, International Society for the Study of Vulvovaginal Disease, 2015, http://www.isswsh.org/images/PDF/Consensus_Terminology_of_Vulvar_Pain.pdf
- Goldstein, Andrew, MD, Pukall, Caroline Ph.D., Brown, Candace, Bergeron, Sophie, Ph.D., Stein, Amy, DPT, Kellogg-Spadt, Susan, Ph.D. “Vulvodynia: Assessment and Treatment”, The Journal of Sexual Medicine, 2016;13:572-590, https://www.sophiebergeron.ca/images/publications/Goldstein_2016_Vulvodynia.pdf
- Weil McCann, Emily. “Towards a better understanding of the lived experience of vulvodynia and its impact upon gender identity: an interpretative phenomenological analysis”, University of Iowa, Summer 2015, https://ir.uiowa.edu/cgi/viewcontent.cgi?article=5937&context=etd
- Cornforth, Tracee. “What Causes Vulvodynia Symptoms?”, Verywellhealth, Oct. 2018, www.verywellhealth.com/facts-about-vulvodynia-symptoms-and-treatment-3521194
- “Female Genital Problems and Injuries.” Michigan Medicine, www.uofmhealth.org/health-library/vagts#hw89443
START YOUR JOURNEY TOWARDS HEALING
Get a weekly dose of resources, tips, and strategies to help you to conquer vulvodynia (and other V conditions).